
Justin Heenan
June 1, 2022, noon
As a Registered Psychotherapist (Qualifying) working with clients with eating disorders, I will be discussing the theoretical approaches to this treatment while also sharing my experiences on treatment approaches such as Mindfulness, Cognitive Behaviour Therapy and Dialectical Behaviour Therapy. I will also briefly discuss Enhanced Cognitive Behaviour Therapy and Interpersonal Therapy. This piece will give therapists an overview of the basic approaches to treatment of clients with eating disorders and the best therapeutic approaches to take in order to give their clients the best possible outcomes.
Theoretical Orientation
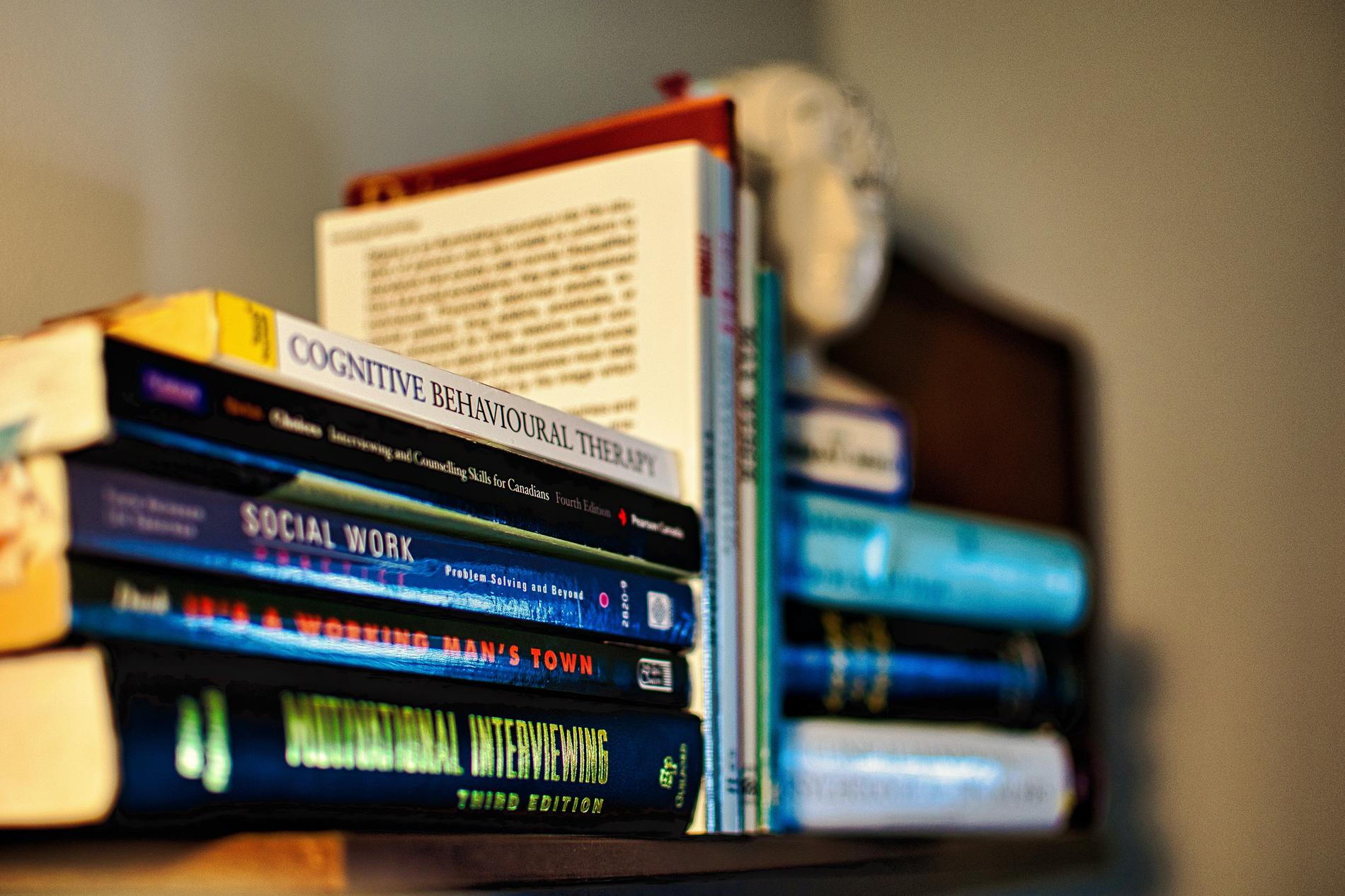
Cognitive Behavioural Therapy
Research suggests that Cognitive Behavioural Therapy (CBT) is quite effective for helping those with issues of eating disorders (Berkman et al., 2015). CBT can be helpful for a variety of forms of eating disorders and clients of various age groups. Clients who exhibit issues of restricting calories, binge eating and purging, and body image issues could truly benefit from CBT (Berkman et al., 2015) (Murphy et al., 2010). However, I am quite cautious of the use of CBT for all of my clients. Many clients who report having an eating disorder will also engage in perfectionism. They may be doing their absolute best on the homework activities to please their therapist and portray the idea of being perfect. For these instances, I may shift my approach to avoid this attachment behaviour. While CBT can be helpful, it may not work for every client.
Mindfulness
Mindfulness-Based Cognitive Therapy is, at times, necessary in this therapeutic relationship in order to stabilize many clients. This can be especially useful in the early stages of discussions with clients around their potential past trauma. By using these techniques, I am able to stabilize and give clients the skills necessary to face their traumatic memories to avoid dependence on destructive behaviours (Dimidjian & Segal, 2015). Many of these mindfulness techniques are used in the short term to help reduce anxiety and the re-experiencing of past emotions.
Dialectical Behaviour Therapy
With many of my clients, using a longer term approach to therapy is often necessary. The incorporation of Dialectical Behaviour Therapy techniques can be very helpful in supporting these clients (McKay, Wood, J., & Brantley, 2007). I have found that along with mindfulness, the incorporation of more work in interpersonal effectiveness, distress tolerance and emotional regulation is of tremendous benefit to some of my clients with eating disorders (McKay, Wood, J., & Brantley, 2007).
A Topical Literature Review
Throughout the years of seeing clients with eating disorders, I have used a number of important and relevant pieces of literature to support me, as a therapist, in treating these complex and varied cases and to support my rationale behind the treatment plans that have been put in place. The current literature points to a clear effectiveness of Cognitive Behaviour Therapy when working with eating disorders (Atwood & Friedman, 2019). Specifically, enhanced Cognitive Behaviour Therapy proves to be quite impactful for clients struggling with eating disorders (Atwood & Friedman, 2019). CBT and E-CBT can have some tremendous impacts on clients who exhibit signs of perfectionism but in practice, as I mentioned, this may not always be the case in practice (Rozental et al. 2018). This needs to be treated on a case by case basis in order to truly support the client.
Mindfulness Based Cognitive Therapy can provide successful outcomes to those who are in crisis (Williams et al. 2006). When discussing past trauma, stabilizing the client can be necessary at times and can be quite helpful in building the therapeutic relationship.
Treatment Options
There are many manners in which eating disorders are treated in a therapeutic setting. If a client expresses potential interpersonal issues, I would consider using an Interpersonal Therapy approach to treating that client (Murphy et al., 2012). However, if I feel as though the interpersonal issues were not the most pressing, I would take more of a Cognitive Behavioural Therapeutic approach. If the client wanted homework, I would examine this carefully as it could be playing into the client’s perfectionist tendencies. Much of the homework I give is centered around behaviour modification and mindfulness techniques (Josefowitz & Myran 2020). Incorporating the unique and specific needs of the client into homework assignment is essential.
In essence, I like to be fluid in my ability to support these unique and diverse clients. The key to this process is understanding your client and what they need to be successful. This comes with building a positive therapeutic relationship early on, while establishing trust and professional boundaries within sessions.
Conclusion
Working with clients with eating disorders has been a highly rewarding experience. I have found that through the process of specializing in this particular area, I have learned a great deal about myself as a professional. Being the therapist that helps them through these challenging issues is a very interesting experience that I have truly appreciated. A major takeaway in these experiences is the need for patience. Eating disorders do not dissipate within a few sessions but rather, these issues tend to be longer term therapeutic processes. Understanding that it is okay that your client does not improve right away is so important. What is most important is that you are there for your client and supporting them through this challenging process, no matter how long this may take.
Author's Bio
Justin Heenan is a Special Education Teacher and Registered Psychotherapist (Qualifying) who specializes in treating Anxiety and Eating Disorders in Private Practice. He takes a Person Centered Approach to supporting both his students and clients. He also uses CBT and Mindfulness in treating clients with various mental health concerns. He is also a Course Instructor at Trent University’s School of Education. Justin is very involved in the Durham Down Syndrome Association and the Special Olympics and he was named the 2021 Educator of the year by Special Olympics Ontario.
Connect with Justin:
justinheenancounselling@gmail.com
https://www.instagram.com/justinheenan/
https://www.youtube.com/channel/UC48N2cYT0fpYqky5_TU0XpA
https://twitter.com/justinheenan
https://www.linkedin.com/in/justin-heenan-6768355b
Works Cited